Confession: I have cried nearly every day since the presidential debate last week.
Why? Because I feel so overcome with frustration and powerlessness when it comes to reproductive rights and procreative liberties.
Politics is never a good choice for my mental health. Perhaps I should choose not to read the news stories. Perhaps I should silent certain accounts on social media. Perhaps I should; but I don’t.
I don’t because I don’t want to be silent on this issue. I don’t want to ignore it.
I am enraged at the way abortion is talked about by politicians and political pundits on the right. And I am devastated at the impact abortion bans are having on the pregnancy loss community, and women and mothers more broadly. I cannot let it go.
Last night I saw Esther Perel speak. She said that political polarization doesn’t happen just because people hold different opinions. Polarization happens when people become so convinced that their opinion is correct that they are no longer able to hold space for a different opinion.
Today I read the story about Amber Thurman, a 28-year-old single mother who died of septic shock because a hospital in Georgia waited too long to perform a D&C after a failed medicated abortion. Then I read an Instagram comment on that story from someone who said that Amber’s death was really her own fault because if she hadn’t taken the abortion pills to begin with, she wouldn’t have become septic. As if Amber deserved to die and leave her 6-year-old son motherless because she chose to end a pregnancy.
Second confession: I may have a polarized point of view because I don’t know how to hold space for opinions like that.
My dad to me I should stop “seeking out these stories.” Should I? Should I insulate myself from stories like these to protect my feelings? Or should I search for more and try and amplify them?
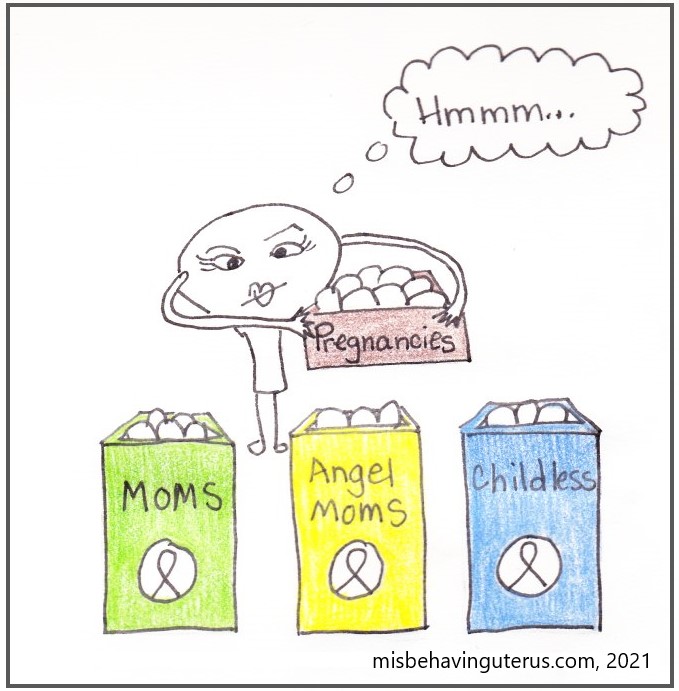
When I was younger (in high school and college), before I had any desire or plans to start a family, I considered myself pro-choice, with limitations. The idea of limitations around “fetal viability” seemed so rational, so middle-of-the-road. The same way I imagine someone might say they are pro-life, with limitations. Exceptions to protect the life of the mother, are so compassionate, so middle-of-the-road.
I now believe that my position was ill-informed and naïve. It was based on my own self-interest, a lack of understanding of how to access care within the healthcare system, and a complete ignorance about the risks and complications that can arise during pregnancy.
In the debate, former President Trump said that some states allow abortions in the 9th month and even after birth. When you hear that, or a term like “late-term abortion,” it sounds terrible. If you picture a healthy woman in her third trimester walking into a clinic where she and a doctor voluntarily end the life of her healthy growing baby, you’d be outraged. What sane person wouldn’t be?
But that’s just not what’s happening. In most instances, a conversation about a later abortion or comfort care after birth is not about whether a baby should live, but about how a baby will die and who should be allowed to make end of life decisions for that child.
I listen to stories like this one from Callie in Georgia and want to scream. Callie was carrying twins but one of the babies had many lethal organ defects. To protect her own health and save the life of her other baby, Callie needed to have a “selective reduction” (a type of abortion), but it wasn’t legal in Georgia so she had to travel to New York for the procedure. The delay in getting treatment caused complications that eventually led to pre-term labor (of her other baby) and sepsis (for her).
Allie Phillips of Tennessee had to travel to a clinic in New York for similar reasons.
A woman I met through my nonprofit work found out her baby stopped progressing in her second trimester. She lived in Texas and had to travel to New Mexico because she couldn’t find a doctor in her state who would perform a D&E procedure (her preferred method to manage her loss) even though her baby was already dead.
I see so many comments on social media or in the comments section of news articles that claim stories like these are hyperbole or that they are irrelevant because they meet the exceptions under the law. If that were the case, these women would have been properly cared for. The laws are insufficient.
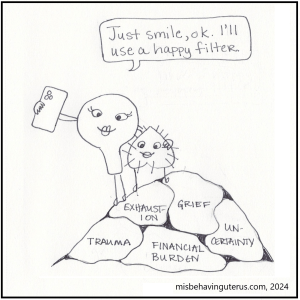
I am aware that I might be too close to this issue to have objectivity. When I read stories about women who have made the choice to end wanted pregnancies, I do cry for them, but I also cry for me. Because I know what it feels like to want a pregnancy so badly and have it end in a way that is outside of your control, and I don’t want that for anyone else. I want to find Callie, and Allie, and all the other women and hold them close and tell them, “This sucks. I’m so sorry, and it’s not fair. What on earth can we do to make this terrible, awful thing just a bit easier for you? What can we do to give you back a tiny shred of autonomy in a situation that is your worst nightmare?”
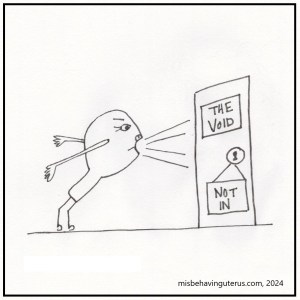
But I can’t do that. So here I sit, sending a blog screaming into the void.
Live Action (which I hesitate to even link to) is a nonprofit organization leading the pro-life campaign. It is well funded, and it is spreading lies.
Live Action claims that removal of a fallopian tube due to an ectopic pregnancy is not an abortion because it does not ‘directly kill the child.’
They claim that the induced labor and delivery of pre-viable baby (in the case of premature water breaking) is not an abortion because it doesn’t ‘target the baby’s body.’
They claim that “necessary medical treatments that are carried out to save the life of the mother, even if such treatment results in the loss of life of her unborn child” are not abortion.
They claim this because they say that abortion is the “direct, intentional killing of an unborn child.”
They purposely frame it this way to play to people’s sensitivities and sensibilities – threading a delicate needle through all the situations in which you might find grace or compassion for those terminating a pregnancy. They are trying to make abortion a dirty word.
But these ARE abortions. Medically.
The removal of an ectopic pregnancy is a type of abortion. A selective reduction in the case of multiples to protect the life of the other baby(ies) is a type of abortion. Induced labor after pre-viable premature rupture of membranes is a type of abortion. The decision to terminate a pregnancy for medical reasons after the discovery of a lethal fetal anomaly is a type of abortion.
It is impossible to anticipate every scenario which might necessitate an exception to a law. Doing so allows us to lose sight of the very real, very difficult conversations about maternal mortality and perinatal and infant death. Pregnancies go wrong. Unexpected complications occur. Not all babies will live. It is a terrible, difficult reality. Sometimes a conversation about abortion is a necessary part of healthcare. And healthcare is a necessary part of LIFE.